A model that works, powered by a decade of trusted experience.
In a healthcare landscape filled with good ACOs, Aledade thrives on being a great ACO.
The right people in charge - you.
Good ACOs use a physician-led model - from their board composition to product development - which outperforms the shared savings revenues achieved by hospital-led ACOs. Our proven approach produces even more.
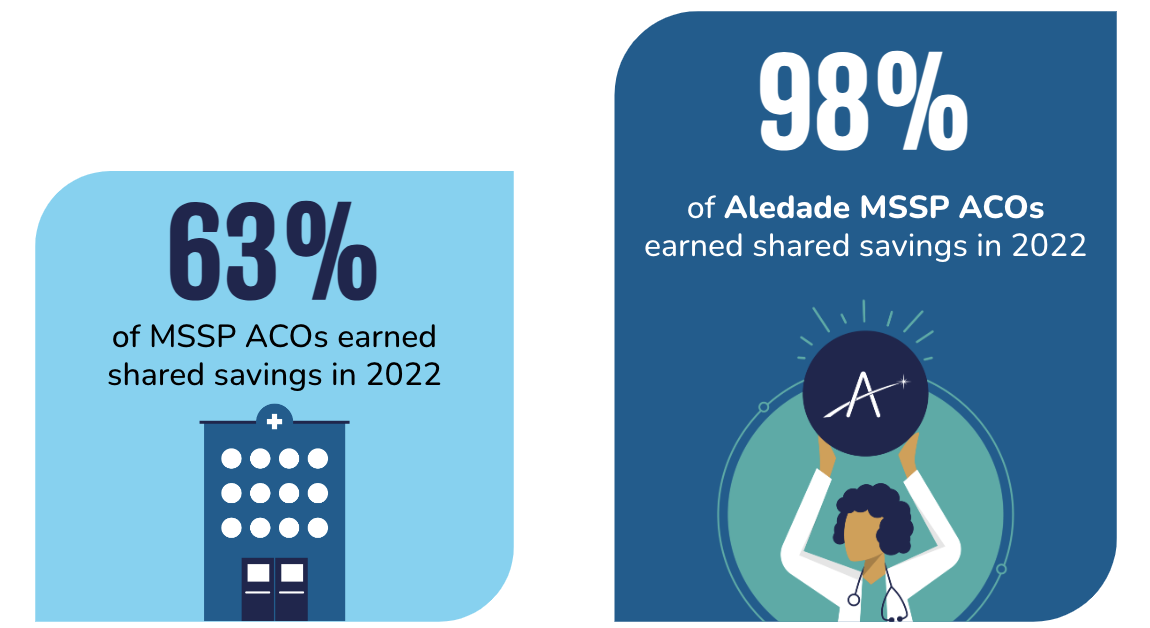
Sustainable track record of success.
Good ACOs can deliver savings once, but our member practices, clinics and health centers do it consistently and improve year after year.

$0
average Medicare Shared Savings Program (MSSP) savings payment per practice

0%
of Aledade ACO members earned shared savings in 2021 (compared to national average of 56%)
$0M
in Medicare Advantage, Medicaid, and commercial savings to Aledade ACOs in 2021
Largest, fastest growing independent primary care network.
Good ACOs have some scale, but our experience and systems enable us to support practices, clinics and health centers of all sizes, across the nation.
Explore our Footprint
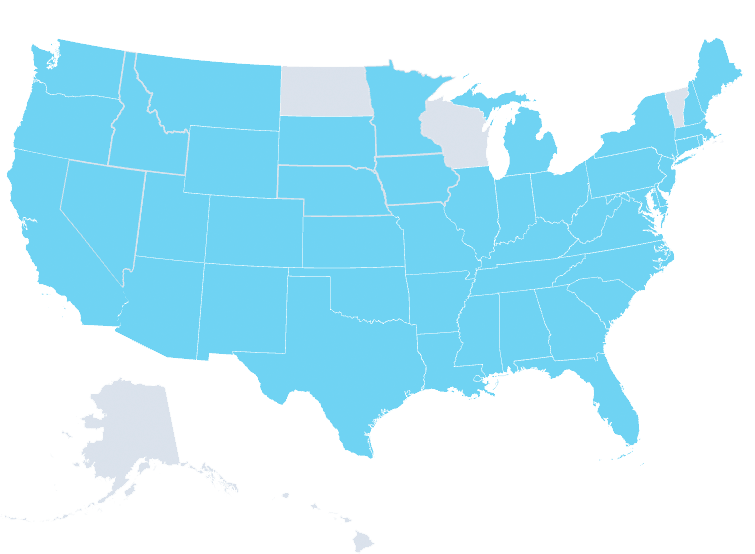

45
States
16,300+
Clinicians
2M+
Patients
1,500+
Practices and CHCs
$20B+
Medical spend
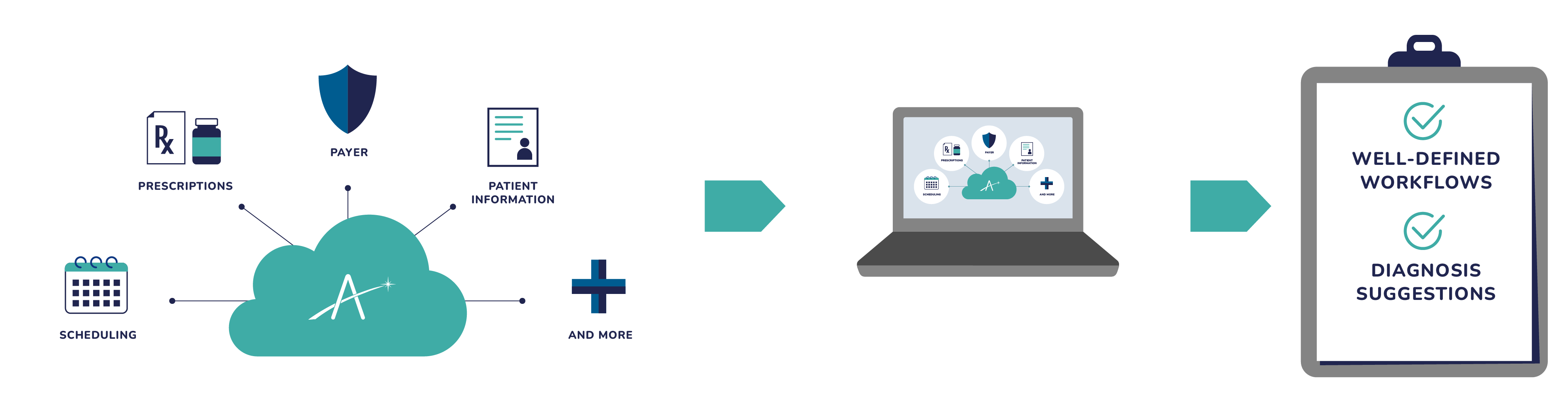
The right information for healthier patients and businesses.
Most ACOs give you access to some data, but we make it easy to identify and solve problems with expanded insights and complementary programs to support and engage your patients.
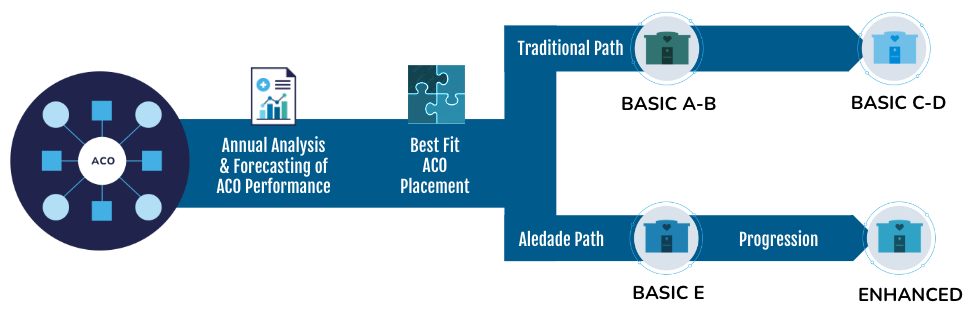
Best-fit ACO placement and downside risk protection.
Good ACOs attempt to take on risk. We go farther by providing 100% downside risk protection and using our data to find the best fit for you, so the ACO can confidently take on more risk for more reward.
Calculate your potential revenues
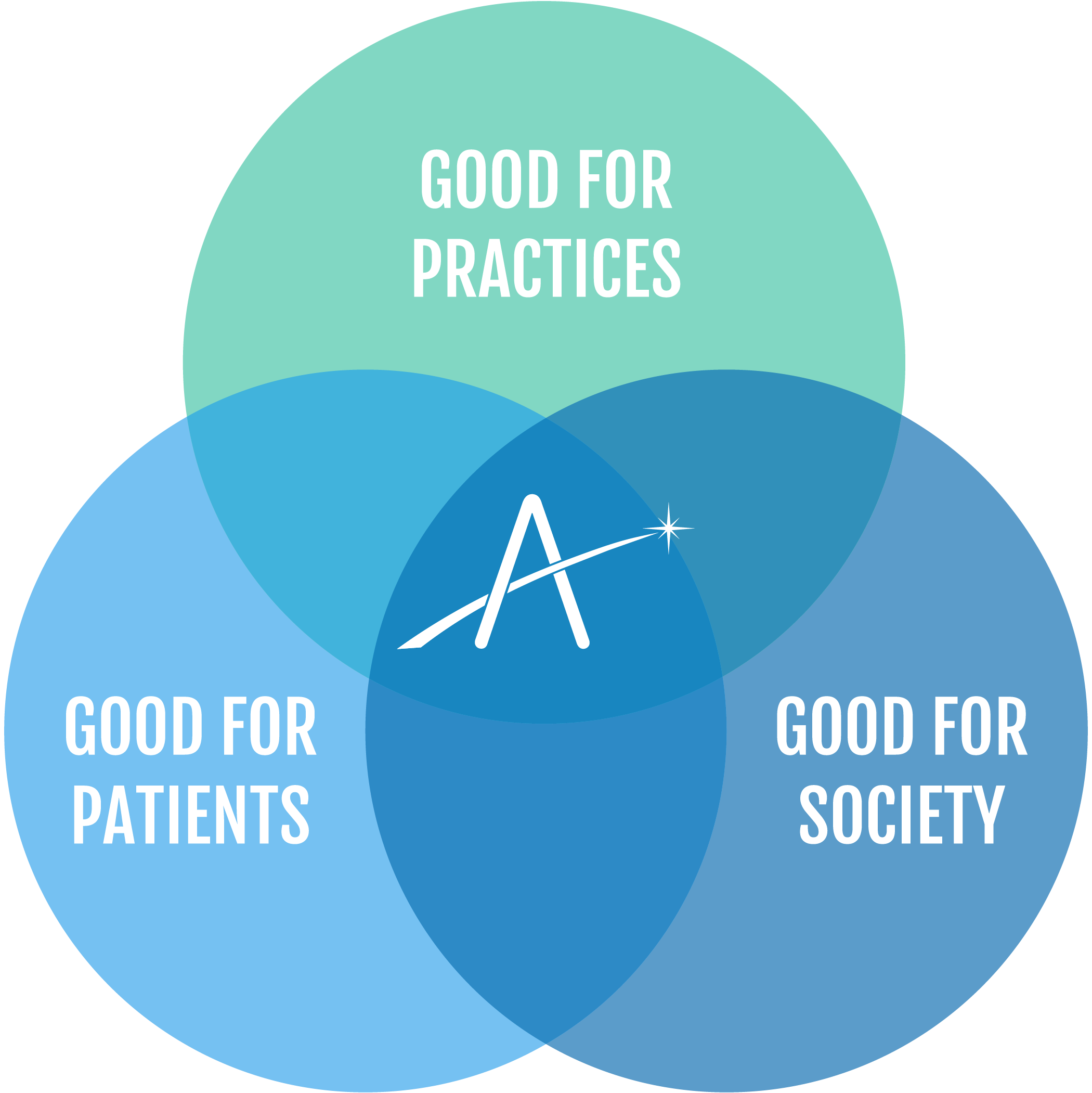
A commitment to our mission.
Good ACOs are mission-centric. We demonstrate our commitment to our mission by embedding it into our corporate legal structure as a public benefit corporation.


A commitment to you.
Empowering primary care to succeed in value-based care models creates healthier patients and communities, at a lower cost for all. When you join our mission and model, you have the advantage of the Aledade Commitment.
Rediscover the joy of practicing medicine.
When you empower your staff with the customized tools, resources and support needed for sustainable financial success and reduced administrative workloads, you can return your focus to what matters most: your patients.
Explore our offering